Too many of us know the drill. After weeks or months of waiting, you finally land a doctor’s appointment. You sit in the exam room, anxious. When the doctor walks in, you get more eye contact with the laptop than with them. The visit feels rushed, and you leave with more questions than answers.
That scene isn’t about indifference. It’s about time. Clinicians are buried under paperwork. Nearly 40 percent of their day is spent on administrative tasks. “Pajama time” has become the norm, with charting and documentation long after shifts end. For every hour spent with patients, two more go into typing, coding, phone calls, or filing.
We often frame the problem as a shortage of clinicians. The faster path is freeing the ones we already have. And that matters when millions of Americans already struggle with limited care access. More than one-third of the country lives in healthcare deserts, where clinics, pharmacies, or hospitals are scarce. In parts of Wyoming, Montana, and New Mexico, picking up a prescription can mean hours on the road. For families in these regions, delays and distance aren’t minor frustrations. They can be dangerous.
The workforce challenges behind those delays are critical. Nursing shortages are worsening, with nearly half of nurses over age 50 and approaching retirement. Physician gaps are most severe in primary care and rural areas. These aren’t abstract numbers; they translate into longer wait times, heavier caseloads, and too many patients who don’t get the care they need when they need it.
Burnout compounds the crisis. Nearly half of physicians report symptoms, and hospitals experience nearly 200,000 nursing job openings every year, projected from today up to 2032. The cost of replacing clinicians is staggering. Every time a nurse leaves, it costs a hospital around $61,000 to recruit and onboard a replacement. A single physician vacancy can drain nearly $1 million in lost revenue and disrupted care. Those losses end up in patients’ premiums, deductibles, and bills.
Hiring alone will not solve this. Training new clinicians takes years. Redeploying the time of current staff can happen in months. And redeployment doesn’t mean shuffling positions on a spreadsheet. It means using artificial intelligence to automate repetitive, manual tasks, while augmenting human expertise, so we can shift large numbers of doctors and nurses back into patient care. It means letting them do the work they went into medicine to do.
Patients already feel the cost of inefficiency. Administrative waste consumes nearly $300 billion every year. That waste doesn’t evaporate; it’s what you see on your statement after a hospital visit or in the premium deducted from your paycheck. National health spending has blown past $5 trillion and is expected to rise to nearly $7.7 trillion by 2032. We’re paying for inefficiency as much as for treatment.
Clinicians themselves are asking for change. A recent Stanford study found that 69 percent of workers across professions want AI to take on repetitive tasks so they can focus on the work that matters most. Doctors and nurses say the same. They don’t want to be replaced. They want to be redeployed. And what they mean is: “Let me give patients more of myself.”
This shift is already underway. Take prior authorization, one of the most frustrating bottlenecks in healthcare. Agentic AI is helping to cut review times from 35 minutes to 17. Across large health plans, that translates into 36,000 clinical hours saved every month, more patient focus, and fewer care delays. Those aren’t abstract numbers. They mean a child with asthma gets her inhaler days sooner. They mean a grandmother waiting for a knee replacement spends less time in pain. Redeployment doesn’t show up as a headline. It shows up in shorter waits, real conversations, timelier care, and better outcomes.
Skepticism about AI in healthcare is fair. Patients should ask if the systems are accurate, if their data are secure, and whether a human clinician is still reviewing the final decision. Those are the right questions. AI should never be a black box. But rejecting it outright ignores the reality: without it, the workforce crisis will worsen. Hiring alone won’t fix burnout or rising costs. Redeploying physicians and nurses through AI-driven efficiency is an emerging lever big enough to matter. Each time an algorithm organizes a chart or summarizes a case, it gives a clinician back the chance to practice medicine as it was meant to be practiced, with patients at the center.
We face a choice. Keep pouring money into inefficiency, accepting longer waits, higher bills, and a workforce stretched to breaking, or recognize AI as the quiet infrastructure that keeps the system working. Think of it like electricity or plumbing. You don’t notice it when it’s working, but without it, everything grinds to a halt.
Redeploying clinicians through AI is not just better for doctors and nurses. It’s better for patients. It means more time, faster answers, and a system that finally feels human again.
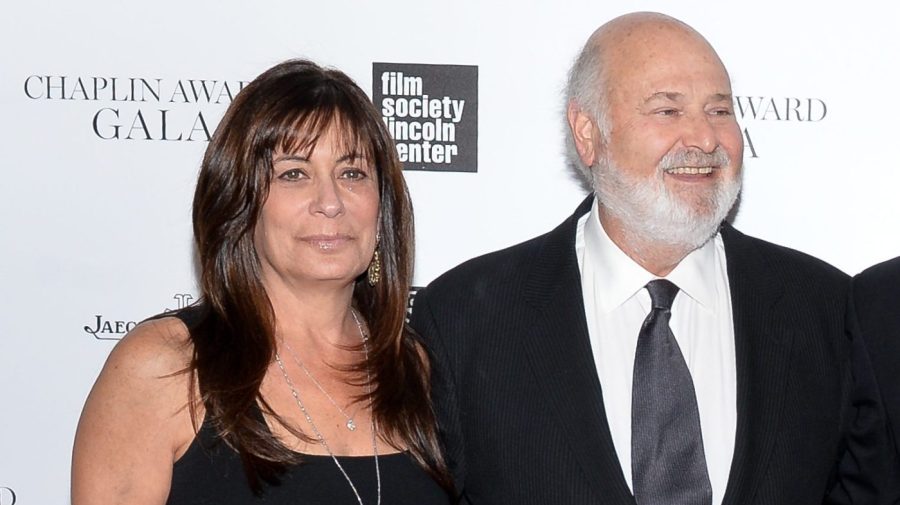
About Joan Harvey
Joan Harvey is the Chair of Growth Advisory Board at Autonomize.AI, a company that uses specialized AI Agents to simplify some of healthcare’s most complex and manual processes, transforming them into streamlined, AI-native operations. Joan is an accomplished healthcare executive with deep expertise in overseeing medical, behavioral, and pharmacy clinical programs, alongside care management services, delivering measurable impact across the industry. Adept at guiding consumer health engagement and behavioral initiatives, with a strong history of developing innovative care solutions that integrate capabilities for health plans, employers, and government programs.