What You Should Know:
– EHR interoperability holds immense potential to improve patient care decisions, enable innovation, and reduce administrative churn. However, a new report from KLAS Healthcare IT Insights reveals that despite advancements in data-sharing technology, interoperability is still far from achieving its desired state.
– The report emphasizes that true interoperability is a team effort requiring healthcare organizations, payer organizations, and vendors to work together to fully realize desired outcomes. KLAS provides an overview of three key EHR interoperability use cases and the challenges hindering data sharing.
Provider-to-Provider Patient Record Sharing
EHR vendors have made substantial progress in their capabilities for sharing patient records, primarily through individual connections, workflow improvements, and large national networks like CommonWell and Carequality. This has made patient data more available than ever.
The Usability Gap
Despite the increase in data availability, KLAS data from the Arch Collaborative shows that clinician satisfaction with external integration has not significantly improved over time. The core issue is the poor usability of shared records.
- Obstacles to Actionable Data: Issues like duplicative data, varying data formats, and poor data mapping prevent clinicians from making the “deluge of data” actionable within the EHR.
- Stagnant Satisfaction: In 2024, only 49% of end-user clinicians agreed that their EHR provides expected integration with outside organizations, a figure that has hovered near 45% since 2018.
Third-Party Application Data Sharing
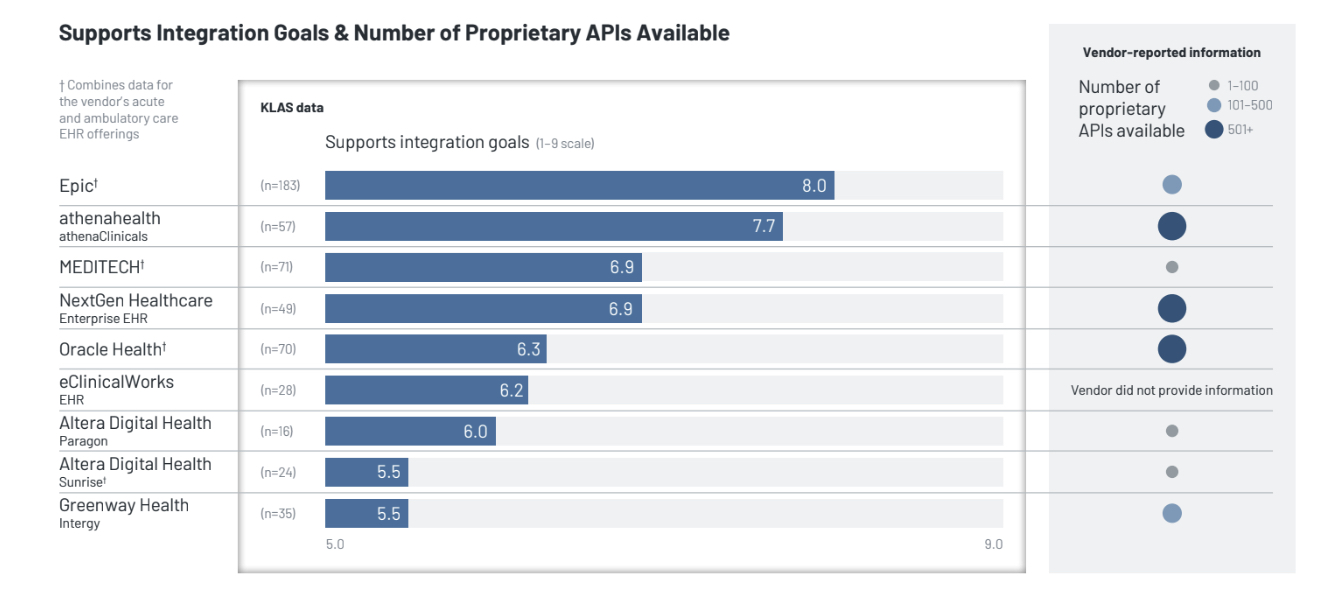
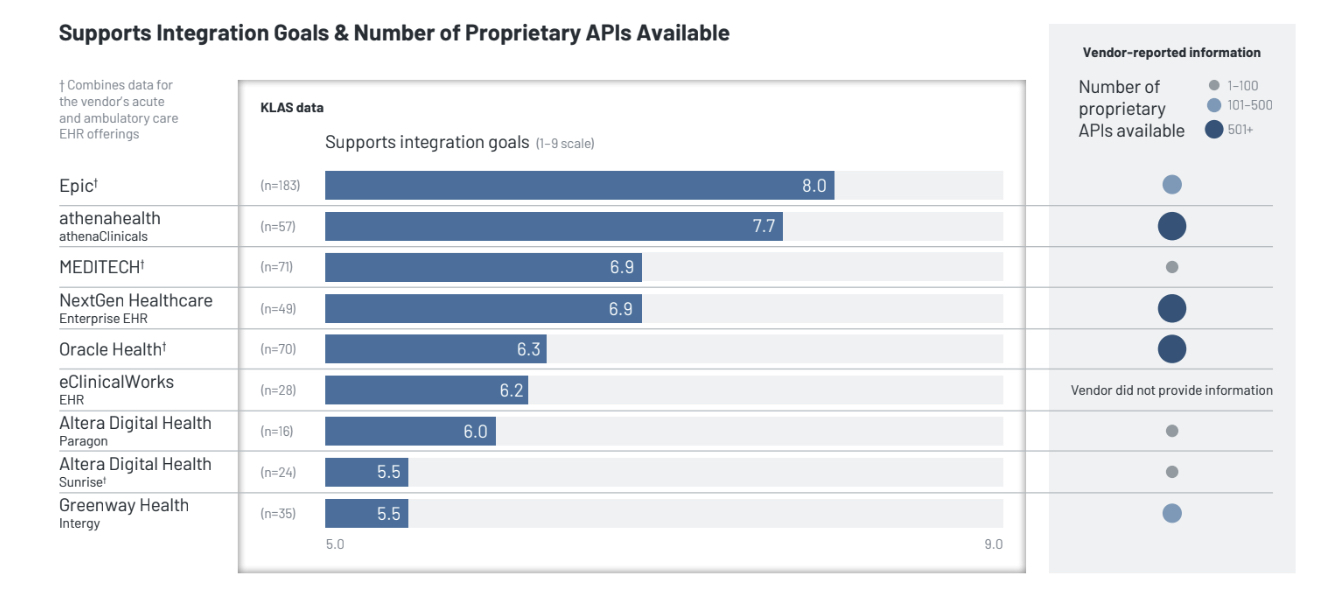
Vendors frequently use the number of proprietary APIs (Application Programming Interfaces) they have available as a measure of their interoperability capabilities. While increased API availability seems appealing, KLAS performance data shows a disconnect:
- API Count vs. Satisfaction: Increased availability of APIs does not correlate with high customer satisfaction regarding a vendor’s ability to support integration goals.
- The Problem of Value: “Having more APIs doesn’t equal receiving more data and value”. Vendors may build different kinds of APIs (single multifaceted vs. several specialized) to achieve the same goal.
- FHIR Limitations: While many vendors report supporting FHIR R4 and USCDI data classes, they still have work to do to ensure FHIR APIs provide the breadth of data that healthcare organizations actually require.
In KLAS performance data, Epic leads the acute and ambulatory EHR offerings with an average score of 8.0 for supporting integration goals, followed by athenahealth at 7.7.
Payer-to-Provider Patient Record Sharing
Data sharing between payer and healthcare organizations remains a long-standing challenge, primarily due to a lack of trust.
- The Trust Deficit: Payers fear fraudulent claims, while healthcare organizations fear giving up too much patient data. This lack of trust contributes to unnecessary administrative churn and costs.
- Regulatory Drivers: Recent federal regulations and CMS mandates (e.g., CMS-0057-F) are spurring organizations to improve data-sharing via bulk FHIR APIs.
- Collaboration is Key: KLAS’s analysis of “Points of Light” case studies found that nearly all mentioned the importance of building trust and partnering (96% of case studies). In contrast, only about half mentioned the need for strong technology (48% of case studies).
The report concludes that while technology is necessary, strong technology alone will not guarantee success; stakeholders must foster transparent collaboration and align goals to achieve a scalable impact on data sharing.