What You Should Know:
– Ushur, a leader in AI-powered Customer Experience Automation for regulated industries, today announced the launch of its Agentic AI solution for provider servicing.
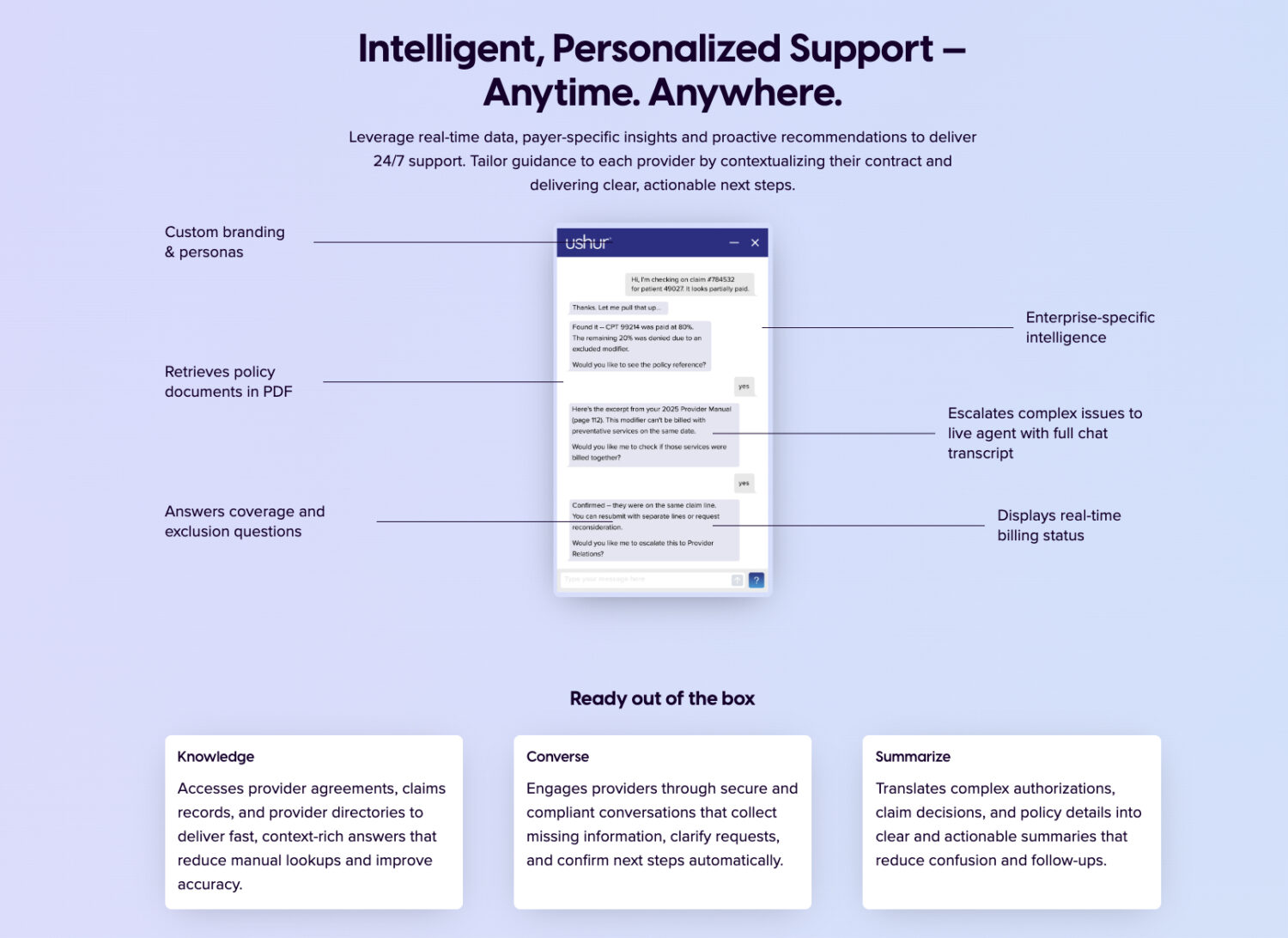
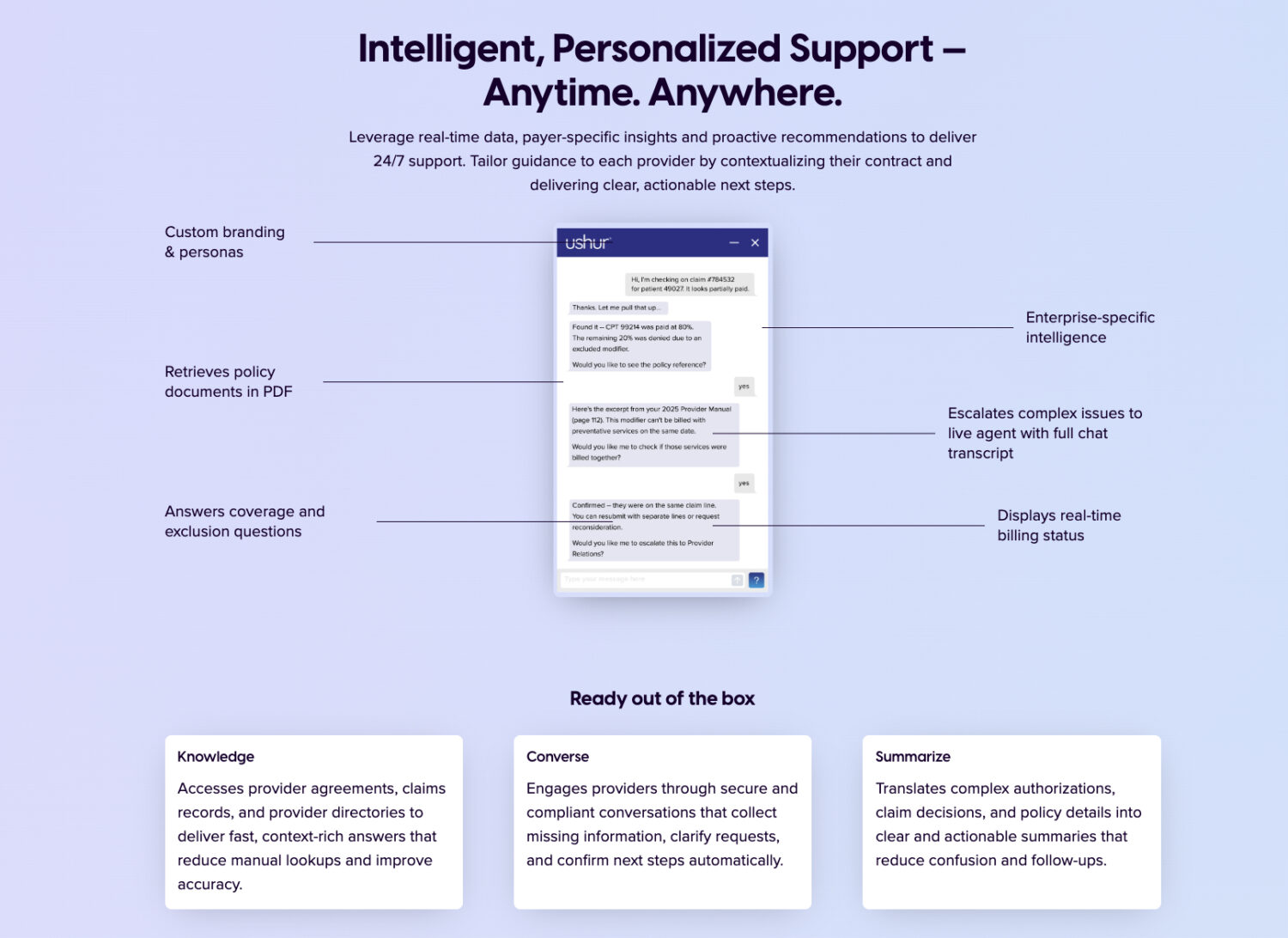
– Purpose-built for health plans’ provider relations, network management, and contact center teams, the solution enables human-like, conversational self-service via voice and chat to answer the most frequent and costly provider inquiries.
Addressing the Provider-Payer Bottleneck
Delays in information exchange between healthcare providers and health plans ultimately impact patients and members. Traditional contact centers often rely on manual, friction-filled processes that erode trust and increase administrative burden. Ushur’s AI Agent addresses this by integrating with core benefits, claims, and credentialing systems to deliver a secure, omnichannel experience.
“Health plans and providers deserve a better way to connect — one that replaces administrative friction with clarity, speed, and trust,” said Simha Sadasiva, CEO and Co-Founder of Ushur. “When providers are supported more efficiently, patients gain faster access to care. This is the next evolution in making healthcare smarter, faster, and more connected.”.
Automating Key Revenue Cycle and Network Functions
Ushur’s solution utilizes domain-specific LLMs trained on healthcare payer language and processes. When deployed as AI Agents, they integrate with core systems to automate critical provider interactions with precision and compliance:
- Benefits Verification: Provides real-time, contract-specific answers to pre-treatment coverage questions, which helps reduce denials and billing disputes.
- Claims Inquiry & Documentation: Automates claim status checks and ingests missing documentation, thereby accelerating adjudication.
- Credentialing & Network Management: Streamlines provider onboarding and directory updates, successfully reducing onboarding timelines and audit exposure.
The Ushur AI Agent for Provider Service enables health plans to deliver consistent, human-like support 24×7, effectively scaling personalized interactions across their entire provider network. This solution is available today as part of Ushur Intelligence.