What are the three sources of liver fat in fatty liver disease, and how can we get rid of it?
Nonalcoholic fatty liver disease (NAFLD) is now the most frequent chronic liver disease, thanks in part to our epidemic of obesity, and is even seen in children. “[N]early 70–80% of obese children may have NAFLD.” Why do we care? Because a fatty liver can progress into fatty hepatitis, which can cause scarring and liver cirrhosis, and cirrhosis is bad enough, but it may also cause the development of liver cancer.
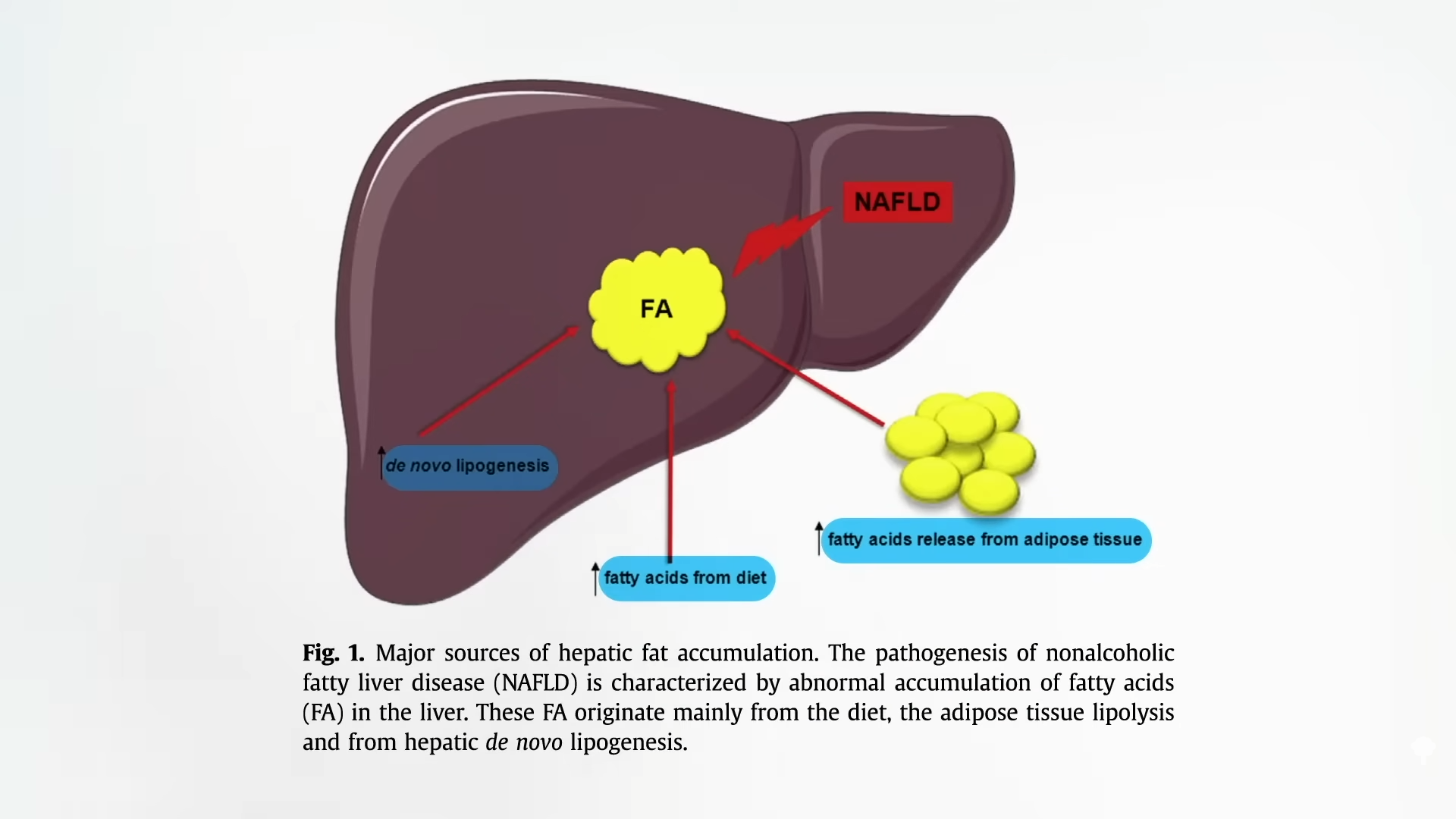
What is the source of the liver fat in fatty liver disease? There are three main sources: the excess sugar in our diet, the excess fat in our diet, and the fat spilling over from our excess body fat, as you can see at 0:51 in my video The Best Diet for Fatty Liver Disease Treatment.
How do we know excess dietary sugar is bad? Because it’s been put to the test. When teens with fatty liver disease were randomized to a diet low in free sugars (meaning a diet low in added sugar and sugary beverages), they experienced a significant improvement within eight weeks. Given these new data, a liver journal editorial read that “a strong argument can be made that we are beyond any period of uncertainty about the harmful effects of excess sugar consumption and that we must now act on the large body of available data to inform the public of the health risks of eating too much sugar.”
And how do we know excess dietary fat is bad? Because it’s also been put to the test. When people were randomized to a low-fat diet or a high-fat diet with the same number of calories, within just two weeks, the liver fat of those on the low-fat diet decreased by 20 percent, whereas it increased by 35 percent in the participants getting the same number of calories but on a high-fat diet.
On the low-fat diet, insulin levels went down about 15 percent, and on the high-fat diet, insulin levels went up about 15 percent. Low-carbohydrate and ketogenic diet advocates often talk about how we need to eat more fat and less carbs to keep our insulin levels down, but the exact opposite happens when it’s actually put to the test. A single high-fat meal not only increases liver fat but also insulin resistance. Within four hours, our whole-body insulin sensitivity can drop by 25 percent, so our body has to pump out that much more insulin. As the accompanying editorial put it: “A single fat bolus [dose] packs a punch.”
So, to help prevent or treat fatty liver disease, patients should limit or avoid eating foods rich in fats. While more long-term clinical trials are always needed, “based on current evidence, we would recommend a diet low in fat, notably in saturated fatty acids, and low in refined carbohydrates, notably by reducing soft drinks consumption…as these nutritional factors may play a pivotal role in NAFLD.” So that means a diet low in meat, dairy, junk, and refined carbs, especially soda. Saturated fat is not only “more metabolically harmful for the human liver than unsaturated fat,” but saturated fat is more harmful than straight sugar. What happened when study participants were overfed with 1,000 calories of saturated fat (like cheese and coconut oil), unsaturated fat (like nuts and olive oil), or sugar (like soda and candy)? Overeating 1,000 calories a day of anything isn’t good for us, but the saturated fat increased liver fat by 55 percent, significantly more than the unsaturated fats, with the candy coming in between the two.
So, “although weight loss is beneficial in NAFLD, certain diets known to induce weight loss can actually cause or exacerbate this disease, and therefore induce insulin resistance, such as very low carbohydrate, high fat diets.” In contrast, “healthy plant-based diets are associated with lower NAFLD risk and more favorable liver function tests profile.” The consumption of legumes (beans, split peas, chickpeas, and lentils), for example, is associated with a lower risk of fatty liver, up to 65 percent lower odds from eating more beans.
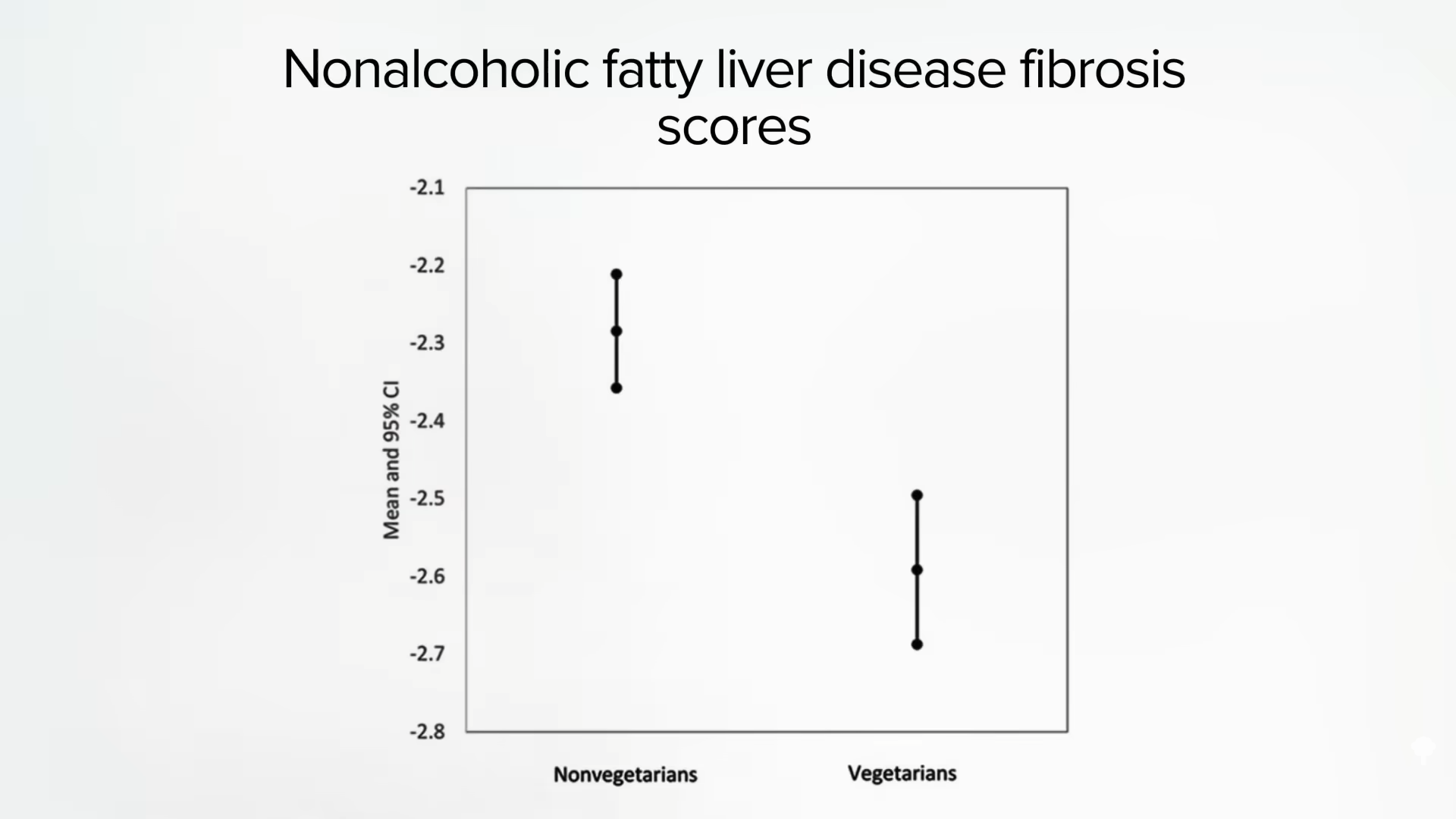
In the earlier study, researchers weren’t looking at people eating strictly plant-based diets, just more or less so. It’s harder to study those eating completely meat-free diets since they currently represent just a small segment of the U.S. population. But what about Americans of Indian descent? South Asians, individuals originating from the Indian subcontinent, are “one of the fastest growing ethnic groups in the United States,” and they appear to largely retain their diets, with about the same percentage of vegetarians as in India—nearly 40 percent. We know that in India, meat eaters are at significantly higher risk of fatty liver disease. It is the same in Taiwan, with vegetarians at significantly lower risk of fatty liver. And even the vegetarians who were affected had significantly less liver scarring, as you can see below and at 4:35 in my video. Their data suggest that “replacing a serving of soy with a serving of meat or fish was associated with 12%-13 % increased risk”—having a single serving of meat instead of soy elevates the risk of fatty liver.
And in the United States? Eating a vegetarian diet was associated with being slimmer and having better blood sugars, better cholesterol, and less than half the odds of fatty liver disease. Is it cause and effect? We have to put it to the test. In an effort to reverse a fatty liver patient’s inflammatory bowel disease with a plant-based diet, researchers found that their liver inflammation was dramatically improved, but they also lost about nine pounds in the first 11 days, thanks to eating healthfully, so it’s hard to tease out the specific effects of the diet on its own. In fact, we have to be careful about rapid weight loss, because all that extra fat being broken down can flood into the bloodstream and sometimes make things worse. So, for individuals with fatty liver disease, losing about three pounds a week might be safer.
Even though a plant-based diet has yet to be properly put to the test in a randomized clinical trial for fatty liver disease, I would submit that it is still the best diet for this disease, and that isn’t based on a single case report, but on the fact that cardiovascular disease, not liver failure, is the most common cause of death among patients with fatty liver disease. And we do have randomized controlled trials proving that a healthy plant-based diet and lifestyle programs can reverse heart disease and open up arteries without drugs, surgery, or stents. Yes, patients with fatty liver disease and fatty hepatitis “may eventually develop cirrhosis [of the liver], but only if they do not die of cardiovascular diseases first.”
Doctor’s Note:
There are some specific foods that may also help. See my videos in the related posts below.
If excess sugar is so bad, what about fruit? Check out If Fructose Is Bad, What About Fruit? and How Much Fruit Is Too Much?.