Pharmacogenomics, also referred to as PGx, is the use of a patient’s genetic makeup to guide safer, more effective medication choices and dosing in everyday clinical practice, including primary care. Although it has emerged as an essential and evidence-based tool in the primary care toolbox, its widespread adoption remains slow.
After more than 30 years in family medicine, I’ve watched every major clinical innovation face early skepticism – from electronic medical records to laparoscopic and robotic-assisted surgery. Yet here we are, firmly rooted in amazing advances in cancer care, rare disease treatment, and new standards in maternal-fetal medicine—all using genetic insights to help guide care. The future is clearly here, but there still remains doubt in the minds of primary care doctors on the place for PGx testing.
The Biggest Myths about PGx and Primary Care Medicine and What the Data Actually Shows
When I speak to family physicians, internists, and nurse practitioners across the country, they share the same quiet doubts: Is pharmacogenomics really relevant to what I do every day? Won’t it take too much time? Can my patients afford it—or will insurers even pay? Much of this hesitation stems from persistent misconceptions about PGx in primary care—and we must examine the research and evidence that dispel those myths.
Myth #1: “It isn’t relevant to my practice”
Primary care physicians are acutely aware that the trial-and-error approach to prescribing is often frustrating to both patient and practitioner, with huge impacts on outcomes, patient safety, compliance, and trust. Some patients metabolize certain medications very rapidly, while others metabolize them poorly, leading to increased side effects and intolerability. Statins, SSRIs, pain medicines, and proton pump inhibitors are just some examples of frequently prescribed treatments with well-established drug-gene interactions (DGI) that influence both tolerability and efficacy.
Here are everyday scenarios where PGx directly improves routine primary care decisions:
- Behavioral health: Doctors tend to choose SSRIs based on personal preference or experience—but these are among the most common medications influenced by genetics. Utilizing PGx testing early in treatment can dramatically shorten the time to remission and decrease the number of “treatment-resistant” labeled patients.
- Pain management: This is often the difficult thorn in the side of primary care physicians. The opiate crisis and specialists’ reluctance to prescribe places an unfair burden on us, and it is our responsibility to prescribe pain medicines effectively and safely. PGx has an important role in determining response to NSAIDs, tramadol, and opiates.
- Polypharmacy and aging patients: Reducing polypharmacy, falls, and cognitive issues in elderly patients is an everyday concern in my practice—and PGx helps identify medications that are more or less likely to be tolerated in this vulnerable population.
- Cardiovascular risk and statin intolerance: Reducing LDL levels to new lows in at-risk cardiovascular and diabetic patients often requires high-dose statins—several of which are influenced by genetics. PGx testing allows physicians to not only choose the best-tolerated medicine, but also convince patients that they are unlikely to experience side effects (often reinforced by internet “research”) because of our careful attention to their unique genetic makeup.
These examples are not theoretical, rare, or irrelevant. On the contrary, they are clinical, immediate, and actionable.
Myth #2: “It’s too expensive”
The reality is that many PGx panels are comparable in cost to panels doctors order routinely, such as comprehensive metabolic profiles and lipid panels. Many are covered by Medicare, Medicaid, or commercial insurance when medically justified, and testing may help with prior authorizations when there have been multiple drug failures.
Let’s address cost further. Adverse drug reactions (ADRs) are the third leading cause of death in the nation, according to recent analyses, surpassing stroke and respiratory disease. Not only that, but conservative estimates place ADRs at $30 billion per year in the U.S. Organizations that have adopted PGx-guided care have demonstrated fewer medication-related hospitalizations and lower overall medication costs. In a value-based care environment, PGx has justified itself as a cost-saving precision tool.
And here’s a mantra that’s often heard when describing PGx testing: “Test once and query often.” Unlike the metabolic profile and lipid panel, the PGx test never needs to be repeated and results can be applied to future prescribed drugs, including those new to the market.
Myth #3: “It’s too complicated”
As I get older (dare I say, wiser), I understand the worries that interpreting genetic results seems daunting. Genetics taught in medical school was minimal and perhaps long forgotten, while advances, concepts, and terminology have certainly progressed significantly. I know, I know… the alphabet soup of terms like CYP2D6 and CYP2C19 are not in our daily lexicon and add to the idea that PGx is not quite ready for prime time. Let me reassure you, though, that utilizing these tests is far less complicated than many other things we deal with routinely. Laboratories provide extremely easy to understand recommendations that are based on FDA guidance, CPIC (Clinical Pharmacogenetics Implementation Consortium) guidelines, or other established sources. Many use a simple “traffic light” system—green for safe, yellow for use with caution, red for avoid.
Myth #4: “It takes too much time and I’m already overburdened”
Incorporating PGx testing into my practice is as simple as ordering any other test. In fact, cheek swabs or saliva-based tests are simpler than blood draws and can be done during a routine visit or mailed to a patient’s home. Think of how ordering Cologuard vs. a colonoscopy is appropriate for some patients and is now part of many of our routine workflows. Often, results can be integrated into the EMR and clinical support tools can be carefully employed at the time of prescribing. The real timesaver here, though, is the elimination of trial-and-error prescribing, patient phone calls regarding ineffectiveness or side effects, and pharmacy callbacks.
Advancing Care With Purpose and Precision
For me, PGx testing represents the essence of compassionate primary care medicine. “Primum non nocere” (first do no harm) was our oath when we graduated medical school. Prevention and patient engagement are what we strive for each day.
As primary care continues shifting toward more personalized and proactive models, tools like PGx will play an increasingly important role in helping us deliver safer, more effective treatment the first time.
As a family doctor, I believe that it is the physicians’ obligation to translate new science into everyday care. Personalized medicine has never been a new catchphrase; it’s what we’ve always strived to attain. Here’s a tool to help. Let’s embrace it.
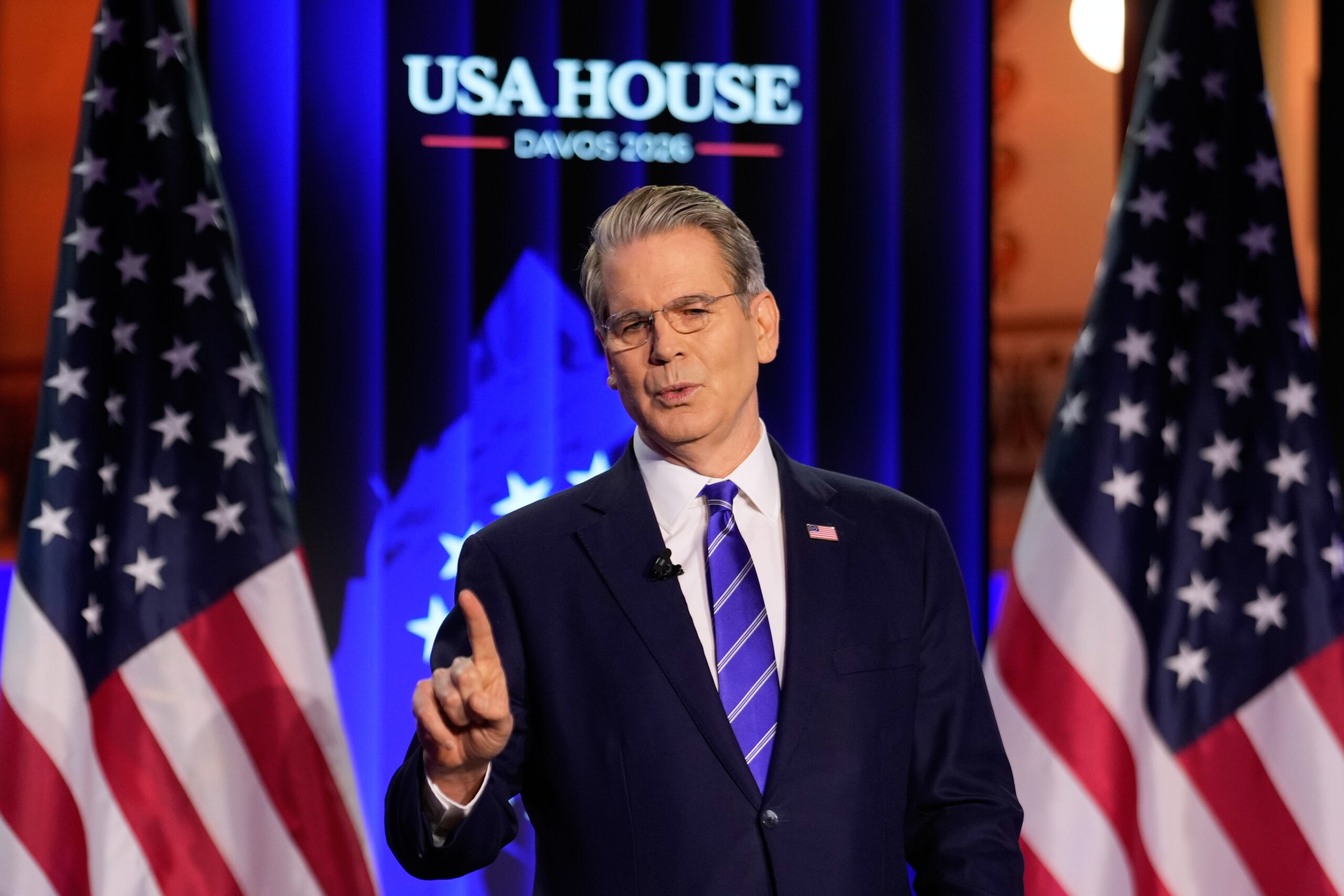
About Dr. Joel Diamond
Dr. Joel Diamond, MD is the Co-Founder and Chief Medical Officer at Aranscia. Dr. Joel Diamond, MD has extensive clinical and technology experience. He formerly served as CMIO and chairman of the Physician Advisory Board at the University of Pittsburgh Medical Center, St. Margaret Memorial Hospital, where he facilitated 100% adoption of CPOE in a community hospital. He helped develop dbMotion, a solution for health information exchange and population health. He is a diplomat of the American Board of Family Practice and a fellow in the American Academy of Family Physicians while continuing to care for patients at Handelsman Family Practice in Pittsburgh, PA.