The Advisory Committee on Immunization Practices’ decision to move away from recommending the universal hepatitis B at birth is being framed as a scheduling change, but it exposes a deeper problem: for more than 30 years, the United States relied on vaccinating millions of low-risk infants instead of building system that identified and cared for the small number of women who along with their babies were truly were at risk. This was performative compassion—a universal policy that looked equitable but avoided the hard work of reaching underserved women.
In the U.S., the route of transmission of hepatitis B to newborns has always been through vertical transmission—pregnant women who have chronic hepatitis B pass infection along to their infants during delivery. A small subset of the population is at risk, but there have been repeated attempts to imply that universal vaccination is necessary because there is real risk for casual transmission. Publications repeatedly emphasize that hepatitis B can survive on surfaces for up to a week and strongly suggest that there is a broad population-level risk. This rhetoric obscures the reality: in the U.S., hepatitis B in pregnancy is rare and overwhelmingly concentrated in two identifiable populations.
Outreach to the women who are at risk requires deliberate action. The vast majority of the 0.9% of pregnant women in the U.S. who have chronic hepatitis B are from areas where the disease is endemic—Eastern Europe, China and Southeast Asia, and parts of Africa. Their point of entry into the U.S. is highly predictable, and importantly, women who immigrate from these countries already get bloodwork drawn for other disease screening; adding hepatitis B would require no new infrastructure, and importantly, would also identify other infected family members.
The other at-risk group constitutes women affected by injection-drug use. Historically, the justification for universal newborn vaccination centered on this smaller group of women and claimed that all babies had to be vaccinated because these women would be unlikely to disclose drug use. But we don’t need to depend on answers to questionnaires to reach them. While these mothers too often get suboptimal prenatal care, they commonly have contact with the medical system, cycling through emergency departments (EDs) for overdose, infections, and trauma. It is routine that hospitals already perform opt-out HIV and hepatitis C for these women, and this represents an easy opportunity for adding automatic hepatitis B testing. The myth that high-risk women “can’t be identified” is outdated and incorrect.
For decades, the U.S. has congratulated itself on protecting infants at birth, but universal vaccination protected the system, not at-risk women and infants. It spared policymakers from building linguistically competent, culturally informed, addiction-aware outreach. A policy sold on equity did the opposite and allowed high-risk mothers to remain invisible.
Among the other justifications for universal vaccination has been the reality that there have been no treatments for hepatitis B. That is changing. Phase 2 and 3 hepatitis B trials are underway and show promising results, and new therapeutics. Identifying high-risk women matters now more than ever, not just for infant protection, but because these women could qualify for trials or be prepared for first-line access to emerging therapies.
The question should not be about whether to move the hepatitis B vaccine from birth to two months; it is whether we will use this moment to finally serve the women who need help. We can redirect resources by adding hepatitis B to immigration screening panels and to existing opt-out ED protocols. We can use EHR flags to ensure follow-up. This is not expensive. It is not complicated. It wouldn’t require new infrastructure. It is not partisan. It would be true compassion for a population that is underserved in many ways, not just in their birth experience.
The universal birth dose was a well-intentioned policy built for a different era. It “worked” but ultimately allowed the system to ignore the women most in need. Changing the infant vaccination schedule without addressing maternal identification will repeat the same mistake, just in a new form. Protecting infants starts with protecting mothers.
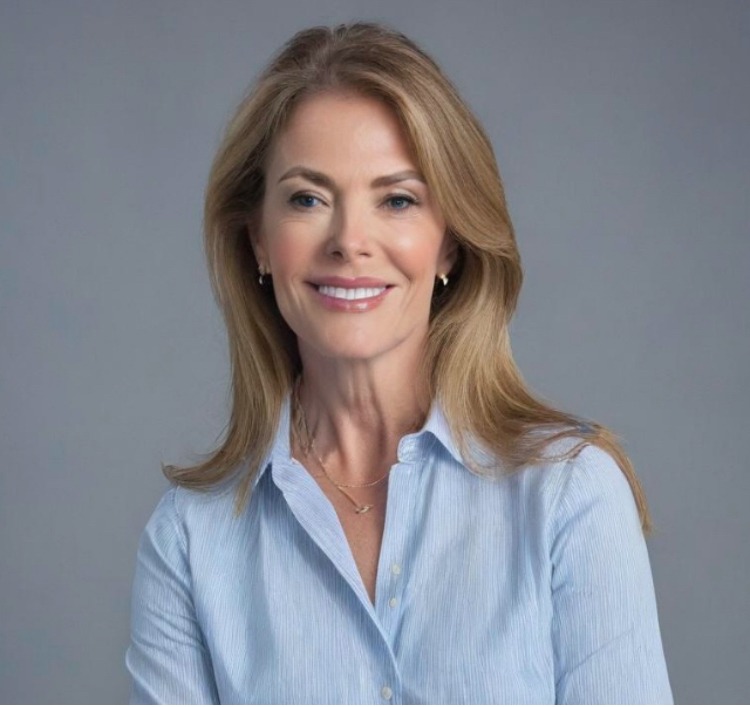
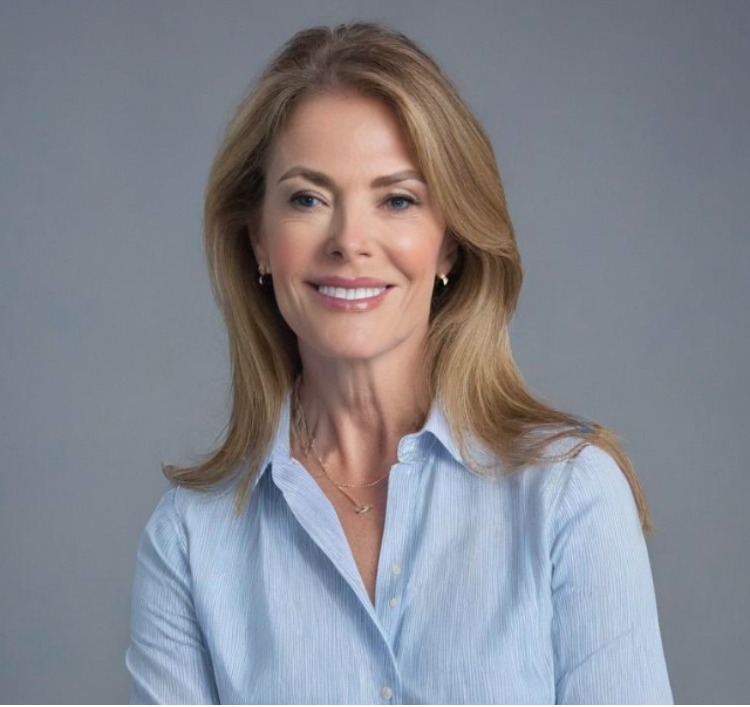
About Monique Yohanan, MD, MPH
Monique Yohanan, MD, MPH is a physician executive and healthcare innovation leader with more than 20 years of experience at the intersection of clinical medicine, technology, and health policy. Dr. Yohanan received her medical degree from the Dartmouth/Brown Program in Medicine and a Master of Public Health from Johns Hopkins. Dr. Yohanan completed her residency in Internal Medicine at Harvard and a fellowship in Geriatrics at Stanford.
Dr. Yohanan is a sought-after speaker on evidence-based medicine, having delivered hundreds of invited presentations including grand rounds at institutions such as Yale and Harvard, as well as at numerous state and national academic meetings. Her published work addresses critical healthcare challenges including pain management, the opioid crisis, and mental health parity.