As healthcare systems confront rising demand for mental health services, digital therapy has emerged as one of the most scalable — and contentious — solutions. Virtual platforms promise to reduce barriers, streamline operations, and expand access. But leaders across health systems and behavioral health networks are beginning to ask more complex questions: What are the clinical limits of online care? Where are the gaps in regulation, infrastructure, and oversight? And how can digital therapy be integrated without compromising therapeutic integrity or patient trust?
Online therapy isn’t a passing trend. Nearly a third of psychologists see all their patients virtually, while 58% use a hybrid model (treating some patients remotely and others in person), according to APA. But, as with any digital shift in healthcare, success depends on strategic design, not just availability.
A Scalable Solution (If Structured Wisely)
Virtual therapy has helped reduce geographic, financial, and scheduling barriers. For organizations serving rural or underserved populations, it’s been a vital expansion tool. Video-based visits have decreased no-show rates, increased appointment flexibility, and allowed providers to serve multiple regions without relocating staff or building out new clinics. For healthcare executives, that’s not just a clinical improvement; it’s a structural advantage.
Evidence shows strong outcomes for common conditions like depression and anxiety when treated online, particularly with structured modalities like CBT. For example, a 2025 study published in Frontiers in Psychiatry found that online CBT significantly reduced depressive symptoms and negative automatic thoughts. And when integrated into system workflows, virtual therapy can become a pressure-release valve for overburdened behavioral health units.
Still, scalability brings new questions. How are therapists trained for virtual delivery? How do platforms ensure clinical quality and safety? And what mechanisms are in place when care needs to escalate beyond the screen?
Risks That Require Executive Attention
While many patients and providers report positive experiences, the digital format introduces operational risks. Nonverbal communication is harder to interpret virtually, making it more challenging to build rapport or detect subtle warning signs. Clinicians report that therapeutic depth and continuity can suffer when sessions are disrupted by technical issues or environmental distractions.
There’s also a growing concern about the erosion of clinical boundaries. Without careful protocols, the home-based nature of online therapy can blur professional lines — a challenge that calls for explicit policy, not just individual discretion.
From a governance standpoint, data security remains a top concern. Platforms handling protected health information must meet strict HIPAA compliance standards, but security doesn’t end with encryption. System-wide safeguards around storage, session recording, and third-party access are essential, especially when expanding virtual services across departments or states.
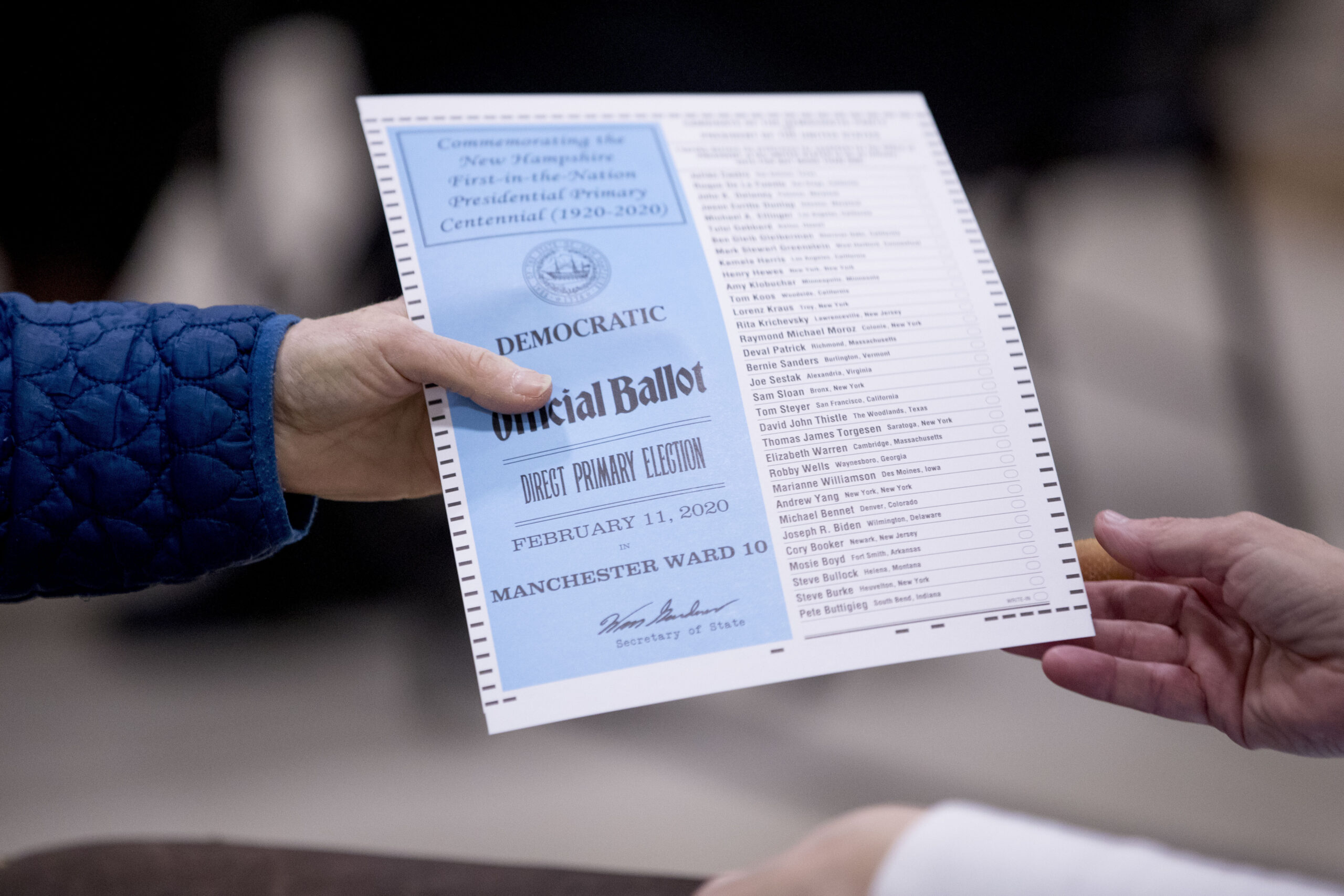
Jurisdictional challenges also complicate implementation. Licensing regulations vary widely, and many states still restrict out-of-state providers despite increasing demand. Executives overseeing multistate operations must navigate a complex and evolving legal landscape to avoid liability while maintaining access.
Clinical Appropriateness and Escalation Planning
No digital solution should be implemented without clear guidelines around clinical scope. Online therapy is effective for stable, lower-acuity conditions, but it’s not suitable for every case. High-risk patients, those experiencing active psychosis, or individuals in unsafe environments may require in-person intervention.
Healthcare leaders need to work closely with clinical teams to define escalation protocols. What happens if a virtual patient experiences a crisis? Are there local resources ready to intervene? Is the therapist licensed in that patient’s state and trained to make that call remotely?
These aren’t hypotheticals. Without operational clarity, what begins as a scalable solution can quickly turn into a high-risk liability.
Rethinking the Hybrid Model
The future of therapy isn’t binary — virtual or in-person — but integrated. Hybrid care models allow patients to move between formats as clinical needs evolve. A system that starts patients with in-person assessments, transitions stable cases to virtual follow-ups, and builds in triggers for returning to physical care can provide both flexibility and safety.
For executives, this means investing in infrastructure that supports seamless transitions: interoperable EHRs, smart scheduling systems, outcome tracking, and platforms that allow providers to document and monitor progress regardless of modality. Hybrid care isn’t just about convenience; it’s about sustainability at scale. Hybrid care offers convenience, as well as a pathway to sustainable, scalable mental health delivery.
Looking Forward: Where Leadership Matters
Innovation in mental health delivery is moving fast, but sustainable implementation requires thoughtful leadership. That includes:
- Standardizing training and supervision for telehealth providers to ensure quality across digital and in-person services.
- Advocating for regulatory reform around interstate licensure and reimbursement parity.
- Collaborating with tech partners to build features clinicians actually need, from digital whiteboards to real-time crisis alerting.
- Investing in analytics to track outcomes, flag disengagement, and improve service delivery based on real data.
Health systems that treat online therapy as a fully integrated modality, rather than a temporary workaround, will be best positioned to meet demand, retain talent, and deliver care that aligns with patient expectations and clinical standards.
Toward a Smarter, Safer Virtual Care Landscape
Online therapy offers a powerful opportunity to rethink how mental healthcare is delivered. But convenience alone doesn’t guarantee quality. Healthcare leaders must weigh the promise of accessibility against the risks of fragmentation, and design systems that honor both innovation and therapeutic integrity.
Done right, virtual therapy can help redefine what comprehensive, patient-centered care looks like in the digital age. But that future won’t be built by chance — it requires the active participation of those shaping the infrastructure, policy, and culture of care.
About Mottsin Thomas, MD
Mottsin Thomas, MD, is a board-certified psychiatrist and founder of bonmente, a comprehensive telepsychiatry practice based in California. His “techie” inclinations started at age 5, when he built a Commodore 64 computer for fun. Since then, he has embraced the value technology brings to modern life but remains sensitive to the importance of human connection, especially in the mental health care realm.