What You Should Know:
– Valerie Health, the AI front office for independent provider groups, today announced a $30 million Series A led by Redpoint Ventures, bringing total funding to $39 million.
– Valerie embeds AI agents with humans-in-the-loop directly inside a clinic’s existing workflows and systems to fully automate rote tasks, including referrals, faxes, and scheduling. This reduces administrative costs by roughly half while improving patient engagement and conversion.
Turning administrative overload into scalable growth
Valerie Health is positioning itself as the AI front office for independent medical practices, embedding AI agents and human experts directly into clinics’ existing systems to automate some of healthcare’s most resource-intensive workflows. By focusing on referrals, faxes, and scheduling, Valerie aims to help independent provider groups improve patient conversion and operational visibility while materially lowering operating costs.
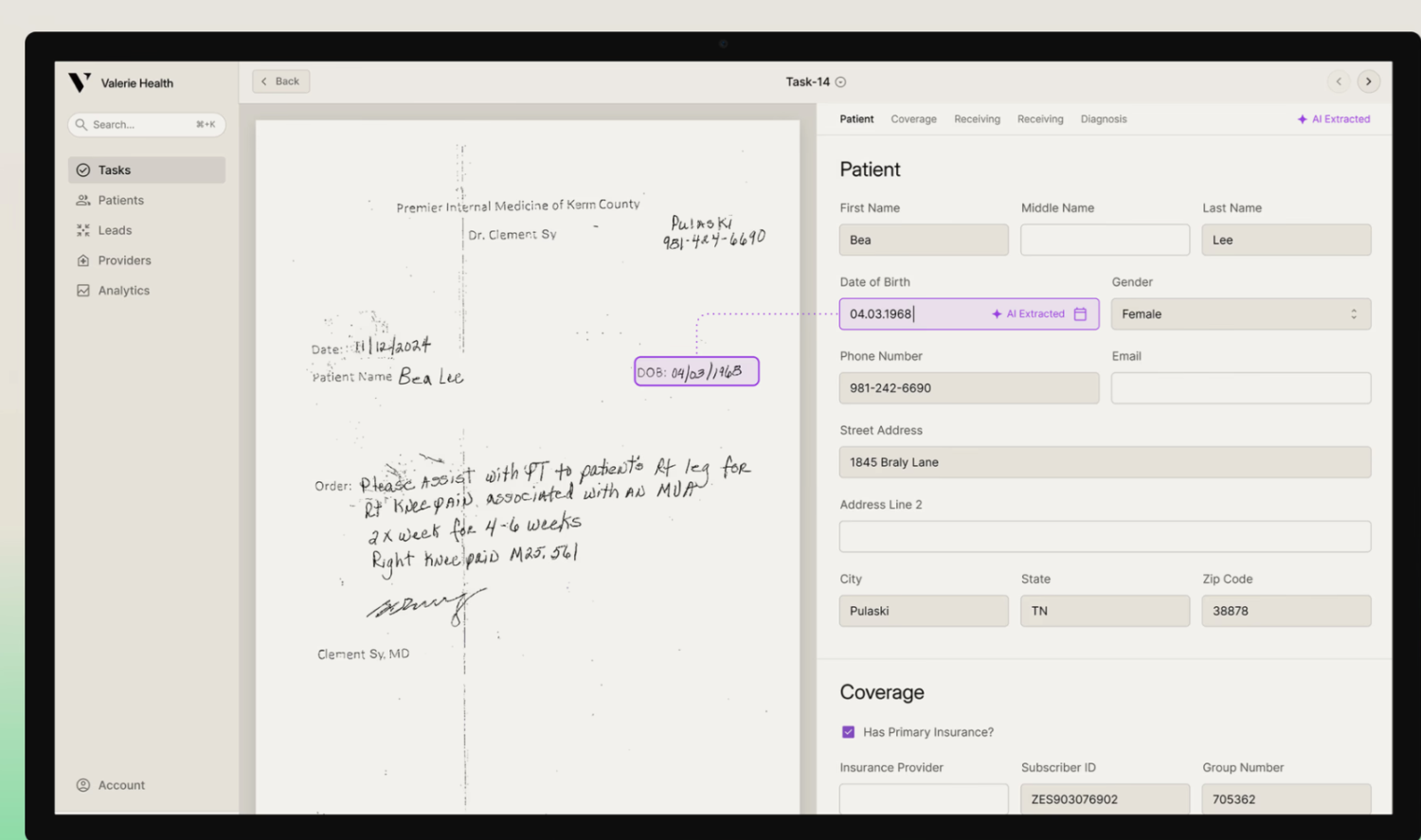
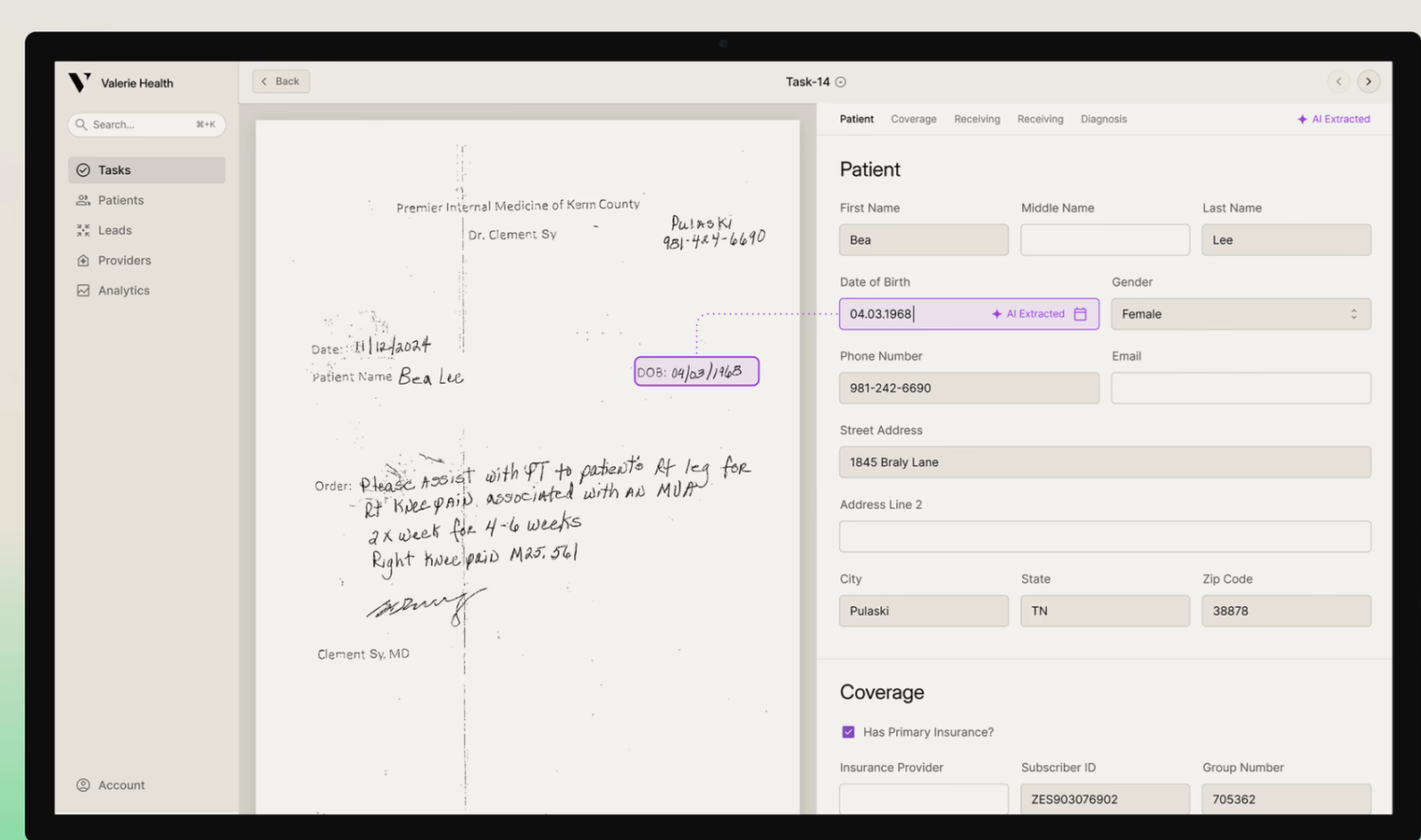
At its core, Valerie addresses a long-standing pain point in outpatient care: the overwhelming volume of unstructured administrative data that flows through front offices every day. Referrals arrive via fax, email, portals, and EHR inboxes, often incomplete, inconsistently formatted, and difficult to track. Valerie’s platform applies large-language-model (LLM) and vision-language-model (VLM) technology to read, classify, and extract structured information from virtually any document format, regardless of source.
What differentiates Valerie is its orchestration layer and review model. AI agents execute clinic-specific workflows, while human experts remain in the loop for review and exception handling. This “AI-plus-human” design delivers near-perfect accuracy within each clinic’s ruleset, converting traditionally manual, error-prone tasks into fast, auditable, and scalable automations that integrate cleanly with existing EHRs and tools.
Valerie already serves large independent physician groups—both physician-owned and private-equity-backed—across cardiology, podiatry, urology, dialysis, primary care, ENT, neurology, home health, and behavioral health. Early customers include several of the nation’s largest provider groups. Over the past six months, the company reports more than 5× revenue growth, including a 3× expansion within existing accounts, alongside the opening of a second office in Chattanooga.
“Independent practices are drowning in paperwork and process, and it’s only getting worse as labor costs outpace reimbursement growth,” said Pete Shalek, co-founder and CEO of Valerie Health. “By acting as an extension of the team—working inside their tools and following their rules—we deliver immediate ROI through faster speed-to-patient, lower costs, and happier staff.”
How Valerie’s AI front office works
Valerie’s platform focuses on three high-impact administrative workflows:
- Referral automation
Ingests referrals from fax, email, portals, or EHRs, completes missing information, and routes them according to clinic rules. Customers report 5–7% higher referral-to-visit conversion rates while reducing handling costs by roughly 50%. - Fax automation
Classifies inbound documents such as prior authorizations, care plans, and record requests, extracts structured data, and synchronizes it directly into the EHR. - AI-driven scheduling
Encodes provider-specific scheduling rules into software and engages patients via SMS to manage end-to-end administrative communication and appointment booking.
Across marquee provider groups, Valerie customers report measurable operational gains: more than 5% growth in new-patient visits, up to 6× ROI, “inbox-zero” referral processing, median referral time-to-entry as low as 19 minutes, and multiple full-time equivalents saved per region.
By transforming the front office from a bottleneck into a growth engine, Valerie Health is making a clear bet that AI—when tightly aligned with real clinical workflows and reinforced by human oversight—can help independent practices not just survive, but thrive.