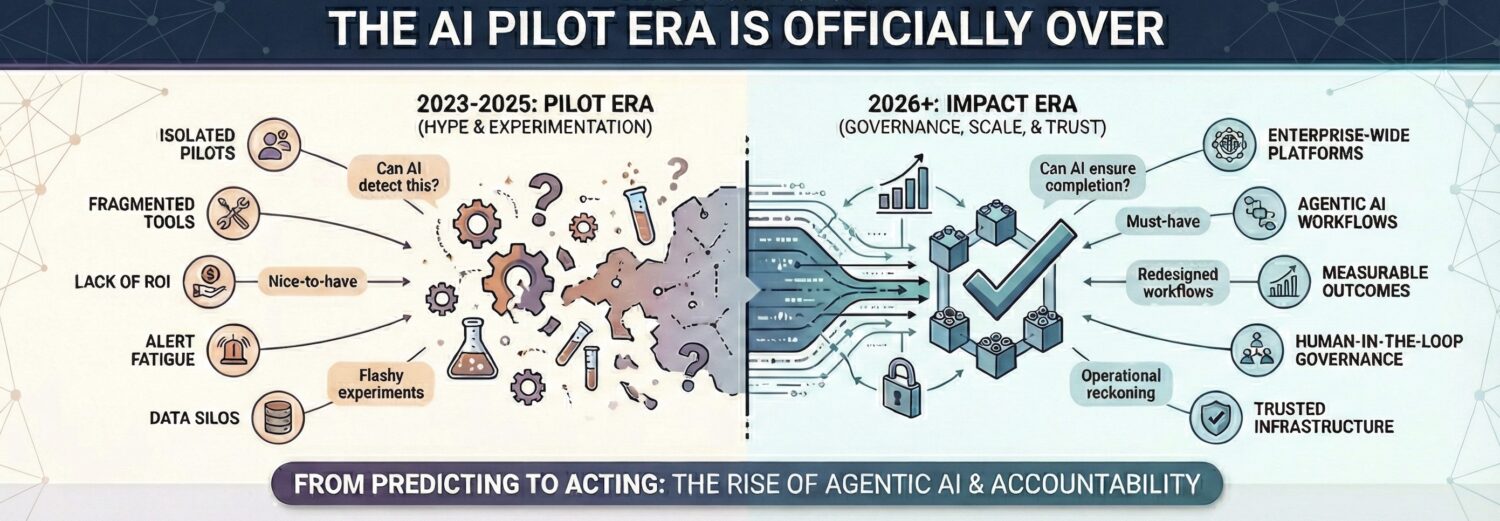
If the last two years were defined by the breathless hype of experimentation, 2026 marks the healthcare industry’s decisive transition from “flashy, one-off experiments” to “top-down programs designed for measurable impact”. Across the digital health landscape, executives agree that the “pilot era is ending,” with the focus shifting entirely to systems that can be “governed, audited, and trusted” at scale.
The narrative for the coming year is no longer about the novelty of generative AI models, but the emergence of “Agentic AI”—tools that move from “predicting to acting” and platform-based workflows where the question changes from “Can AI detect this?” to “Can AI ensure this is completed?”.
From the “invisible” integration of AI into clinical operations to the hard reality that organizations must “redesign our workflows” rather than merely speed up broken processes. As we look toward 2026, healthcare executives forecast a year of operational reckoning, where success will be defined not by technological capability, but by the “hard work required to make AI meaningful.

Angela Adams, Chief Executive Officer of Inflo Health
A new category will emerge: AI platforms that govern other AI, orchestrate workflow across care settings, and guarantee that every flagged finding is routed to a completed action. The question changes from “Can AI detect this?” to “Can AI ensure this is completed?

Maria Ebro Andreasen, EVP & Chief Strategy Officer, FUJIFILM Biotechnologies
In 2026, AI and automation will improve productivity across biopharma manufacturing, with operation improvements and increased asset utilization. We expect to see more facilities add local intelligent autonomous process units, which can provide automated trending, anomaly detection, and insights to speed up investigations and reduce deviations. The result is faster, more predictable compliance and safer products.
Beyond the manufacturing floor, AI-driven automation will streamline administrative workflows to refocus specialized talent throughout other areas of the organization.
Another advancement is the continued expansion of predictive and preventative maintenance. By fusing sensor data with AI-assisted models, teams can forecast equipment service needs before failures occur, increasing uptime and protecting batch success.
Together, AI and automation will raise speed, quality, and resilience across the entire manufacturing value chain and further close the gap in access to medicines.

Dr. Colin Banas, Chief Medical Officer at DrFirst
“We’re already seeing AI move beyond documentation into actual clinical decision support. This is especially impactful upstream in the prescribing process, where AI can surface formulary requirements and coverage criteria before the prescription is even written. That’s a game changer for physician practices and pharmacies because it prevents the interruptions that get in the way of patient care—pharmacy callbacks, PA coordination, all that back-and-forth. Instead of just processing problems faster, this type of innovation can prevent them in the first place.”

Sina Bari, AVP of Healthcare and Medical Artificial Intelligence, iMerit
In 2026, AI will continue its march from nice-to-have to must-have for both healthcare providers and health systems. The FDA has already cleared dozens of new AI-powered medical tools across areas like radiology, cardiology, and gastroenterology, underscoring the technology’s rapid adoption in clinical practice. Marketplaces will start to emerge for competing algorithms, and the provider’s role will evolve into mediating which tool to utilize. Yet the most important currency, patient trust and buy-in, will bring with it the unmet challenge of systematic AI governance. Human-in-the-loop (HITL) systems acting as truth engines will ensure that algorithmic insights are grounded in clinical expertise, free of bias, and resilient to model decay. Advances with compute alone will begin to plateau, and developers will need to engage increasingly sophisticated systems to capture expert human insight and decision making across longitudinal and multimodal data streams.

Frederik Brabant, Chief Strategy and Medical Officer at Corti
Safe AI will expand into underserved clinics
“The clearest opportunity for AI isn’t in the highest-resource hospitals- it’s in the places where clinicians have the least time, the least staffing, and the least access to specialists. When systems are multilingual, low-bandwidth, and reliable in noisy, unpredictable environments, they can materially raise the quality of care in rural and understaffed clinics. In 2026, we’ll start seeing outcome improvements driven by extending safe AI into these underserved settings.”

Amy Brown, CEO and founder of Authenticx
“I see a great reckoning ahead, where business leaders will be asked to show the real proof points for investing in AI. There is no easy button to get AI that’s well-trained and truly relevant to your business use cases. The organizations that succeed will be the ones willing to do the hard work required to make AI meaningful.”

Robert Connely, Global Market Leader for Healthcare at Pega
Practical Gen AI Results Will Surface in Healthcare: 2026 is the year that generative AI will finally move past hype and see practical returns in healthcare. The days of flashy, one-off experiments will give way to top-down programs designed for measurable impact. The focus will shift from isolated pilots to governed, organization-wide AI strategies that improve speed, accuracy, and outcomes across the board. Agentic AI, once envisioned as futuristic “digital coworkers,” will show up instead as practical work tools that quietly streamline processes, guide staff, and drive real business value.
The story won’t be about what AI can do, but what it’s actually doing to make healthcare work better. For example, instead of replacing human agents, generative AI will augment their efforts serving as “co-pilots” doing the research, documentation, and follow-up freeing the agent up to engage the caller. The same pattern is seen with doctors that evaluate a patient’s clinical criteria to make decisions about treatments or medications. AI is used to collect information quickly to enable the provider to make the most informed decision. As the focus of AI evolves beyond experimental initiatives, the ability of generative AI to reduce costs and errors while increasing capacity is driving the opportunity – not the newness or coolness of the technology.

David DeHommel, VP of Payer Strategies at Reveleer
AI Pilots Will Finally Shift to Real-World Deployments With Measurable Impact
Financial pressure will push payers to move beyond experimentation and deploy tactical AI tied to clear ROI, such as risk adjustment and Stars optimization, to increase revenue and reduce costs.
David Everson, Senior Director of Solutions Marketing at Laserfiche
Agentic AI and cloud resilience will be key to drive healthcare efficiency: In 2026, emerging technologies will focus on empowering, not replacing healthcare staff. Interoperability and secure cloud infrastructure will be critical for data continuity, disaster recovery, and protection against ransomware. Agentic AI will transform documentation and care coordination, reducing burnout and enable faster follow-ups. Together, these innovations will create a more connected, resilient, and efficient healthcare system built around both performance and patient experience.

Sachin K. Gupta, Founder and Global CEO, IKS Health
AI and AI’s future
In 2026 we’ll see continued development of a platform approach enabled by agentic interconnected workflows with appropriate human-in-the-loop. There will be recognition that AI is much more of a platform play than the point solution oriented approach that healthcare IT and health systems have traditionally taken. That platform play is going to be deeply enabled by interconnected agentic workflows. These workflows will truly demonstrate that the value of the whole is much greater than the sum of the individual parts, especially when chores of health care are delegated to a platform that alleviates the burdens on caregivers and their care teams.
There is a bit of pragmatism starting to develop around the need for AI to, at the very least, be supervised, but in some cases be assisted by a strong human-in-the-loop so that it is able to completely and safely delegate tasks. There are early signs of a disillusionment trough emerging for certain aspects of AI. AI supervised by humans will start to become much more meaningful as it relates to true assistance, decision making, and clinical decision support at the point of care for the clinical care teams.

Ian Fisher Head, Development Analytics at IQVIA
Drug Development Strategy & AI Enhanced Decision-Making
For drug development teams, a greater weight will continue to be placed on scenario-based target product profiles to guide early strategy and investment decisions. A part of this shift includes utilizing AI to model multiple benefit and risk pathways and to compare how different trial designs may perform under evolving regulatory expectations. Additional scenario variables that drug development teams must account for are the overall patient burdens, unmet needs and access considerations. These factors will be essential in developing plans reflecting what patients and payers value most.
From a regulatory perspective, there are growing expectations that rising FDA workloads will pressure organizations to prioritize transparent trial designs that align more tightly to precedent. In conjunction with this approach, development groups will use AI to analyze historical decisions and forecast the level of evidence needed to secure approval without rework or delay. This approach should result in strategic planning that is more comprehensive and forward-looking, with cross-functional contributors developing a unified narrative from the start.

Lance Hill, founder and CEO at Within3
By 2026, we’ll see AI interfaces sitting on top of all enterprise data, inside and outside the organization, becoming completely commonplace.”

Oliver Kharraz, Founder and CEO, Zocdoc
AI’s Healthcare Race: Offer the Best Patient Experience or Fall Behind
As AI platforms race to manage everyday tasks—from ordering groceries to booking travel—they will need trusted, domain-specific partners for high-stakes transactions like healthcare. Rather than building bespoke services, leading AI players will look to plug into best-in-class infrastructure. Healthcare access is too complex to improvise and too important to get wrong. We will see a wave of strategic partnerships, where general-purpose AI agents outsource healthcare navigation to trusted experts.

Melvin Lai, Senior Venture Associate, Silicon Foundry
Healthcare Holds AI’s Strongest Runway, If It Can Unlock Its Data
Investment may increasingly shift toward fueling new human insight and the systems that preserve it. While most industries face data exhaustion, health tech remains uniquely advantaged, sitting on a vast, still-untapped trove of medical records, clinical notes, and real-world evidence. As AI models in other domains begin to plateau from recycled training data, healthcare has the rare opportunity to keep improving by responsibly unlocking, structuring, and digitizing the knowledge already within its walls.

Dr. James Lu, co-founder and CEO of Helix
In 2026, health systems that have successfully integrated AI into genomics will have a competitive advantage. AI systems can interpret genetic testing results and provide clinical recommendations within hours rather than weeks, enabling genomic data to influence real-time treatment decisions in oncology, pharmacogenomics, rare disease diagnosis and more. Hospitals and health systems that recognize AI-powered genomics will be able to more quickly achieve precision medicine at scale and propel future growth.

Scott Lundstrom, Senior Healthcare Industry Strategist, OpenText
AI in Healthcare Moves from Potential to Proven Impact
AI has long promised to transform healthcare, but most organizations have lacked the tools, governance, and secure data foundations to do it safely. That is beginning to change as clinical-grade AI becomes embedded in core systems like EHRs. By 2026, natural language processing and predictive modeling will support faster decision-making at the point of care, while ambient intelligence automates documentation and reduces administrative load. The shift to proactive, AI-enabled care will depend on building security, usability, and trust into every layer.

Chris Luoma, Chief Strategy Officer at GHX
Agentic AI will usher in the era of prescriptive supply chain orchestration: AI agents will move from predicting to acting, automatically triggering replenishment, contracting, and supplier diversification, creating a proactive, intelligent supply chain ecosystem.

Dr. William Morice, CEO at Mayo Clinic Laboratory
Rapid AI evolution and augmented diagnostics. AI capabilities are advancing so quickly that by late 2026, available tools will look dramatically different from today’s. Exploration of augmented diagnostics and how humans and AI collaborate will compound to determine when to keep or remove the human from the loop.

Dr. Nikhil Nadkarni, child and adolescent psychiatrist, and chief medical officer at Brightline
“AI is going to fundamentally change the digital health market next year, both in terms of digital health operations, and digital health care quality. In terms of digital health operations, AI will move into the background and become a foundational silent hero under the hood. The real value of AI will be in its invisibility. The goal isn’t just automation; it’s the elimination of entire tasks using AI. This is in contrast to the explicit “click here to use this awesome AI feature” user interaction that we often see today.
As for digital health care quality, leading companies will use AI to unlock the creativity of their clinical teams to make their patient interactions more effective and higher quality than what is possible right now. This can come in many forms, from hyper-personalization of content and treatment plans to new tools and interventions. The standout companies will be those that integrate AI thoughtfully, ethically, and in line with care guidelines to truly elevate care quality.
For the overall digital health market, expect to see a proliferation of niche digital health care tools and offerings, followed by rapid consolidation.”

Dr. Aaron Neinstein, Chief Medical Officer at Notable
AI-first practices will reshape care delivery. New practices will be built from scratch around AI Agents to support panel sizes three to five times larger at equal or higher quality and dramatically lower cost. Human connection will take center stage again; AI will handle pattern analysis and routine adjustments, so clinicians can shift from memorizing facts to focusing on meaning – gaining the time and capacity to ask questions like “How does your illness affect your life?” Because of this, nurses, MAs, and care coordinators will move up the value chain, as they can spend more time on empathy, clinical judgement, and complex situations rather than administrative tasks.

Kurt Roholof, CTO at Duality Technologies
Healthcare AI: Local Control, Global Intelligence
Governments and health systems will assert control over where patient data resides, how it’s processed, and who can access it for AI development—yet this won’t mean closing borders to innovation. Instead, leading healthcare organizations will deploy privacy-enhancing technologies that allow clinical insights and AI model improvements to flow across jurisdictions while patient records remain firmly anchored within their country of origin. This will enable global healthcare AI systems to learn from distributed datasets spanning multiple nations, all without a single medical record crossing borders. The healthcare AI winners will be those who master this balance: delivering the collaborative power of worldwide data while giving each nation complete authority over its citizens’ health information.

Abhinav Shashank, Co-Founder and CEO at Innovaccer
When healthcare transitioned to the digital space, we essentially took what we were doing on paper and converted it into digital workflows. As a result, we now have an abundance of technology in healthcare, but everything has become more complex, because now it’s done digitally and faster, not necessarily better. AI, in my view, has the potential to go in one of two directions:
It could make bad processes worse, just faster, which would be disastrous. We’d see poorer outcomes, more administrative burden, and a chaotic system filled with countless agents working against each other.
Or, we could take a transformative approach and redesign our workflows around this technology. Organizations that do this will fundamentally transform, reducing waste, improving margins, and delivering better outcomes. If we merely use AI to speed up existing processes, we’ll end up with a massive increase in costs instead of reductions.
People are already getting tired of AI. Because of all the hype coming from Silicon Valley, not just customers, but everyone, is starting to feel fatigued. Even in the stock market, you can see the signs: predictions of a potential crash are emerging.
AI is a fundamentally important technology, but we’ve overhyped it to a point where the natural adoption curve isn’t being allowed to unfold. Like the internet or other major innovations, AI needs time, five to ten years, for meaningful adoption. Right now, everyone’s agenda seems to be, “What did you do with AI?”, and that obsession could be more harmful than beneficial.

Scott R. Schell, MD, PhD, MBA, Chief Medical Officer, Cognizant
Artificial intelligence has moved past the experimental phase. The coming year will test whether healthcare and life sciences can make AI trustworthy, useful, and human-centered at scale.
A recent Forbes analysis citing Menlo Ventures reports that healthcare is adopting AI at twice the rate of the broader economy, with only about 20 percent of organizations currently using it. That acceleration affirms our previous observations: the pilot era is ending. The next measure of success is not whether AI works, but whether it can be governed, audited, and trusted to serve both patients and progress.
The near-term productivity lift will come less from diagnosis and more from documentation and workflow improvements. Ambient scribes, smart scheduling, and denial-prevention tools are already reclaiming hours for clinicians and support staff. In life sciences, generative systems now draft clinical protocols, summarize literature, and flag pharmacovigilance signals. Individually, each task may seem small, yet together they return time, attention, and morale.
The best systems disappear into workflow. They make existing infrastructure breathe again.

Dr. Thomas Schenk, Chief Medical Officer at Paradigm
“Some of the most exciting innovations we’ll see gaining traction in 2026 are those that meaningfully improve outcomes while helping health plans manage costs. We’ll continue to see the evolution of GLP-1 therapies, along with a growing set of companion solutions designed to help plans better manage the associated spend. At the same time, new approaches to controlling surgical costs are emerging, and AI is opening the door for plans to engage members in smarter, more impactful ways, helping to provide the context and insight people need to better understand their health and make confident, informed decisions. These advances hold tremendous promise for both patients and the health plans that serve them.”
“As we head into 2026, health plans are under immense pressure, and that strain is likely going to deepen. We’ll see plans continuing to adjust their case and market mixes, cutting administrative costs wherever possible and doubling down on the programmatic levers they rely on when they’re searching for stability. Some will push automation even further to try to be more aggressive on cost containment. These are the moves we can expect before any meaningful relief arrives.”

Mike Sitzman, partner at McDermott Will & Schulte
The AI-Generated IP Crisis—Is it Patentable? – “While the foregoing advancement will be hugely important and beneficial in the world of healthcare, they pose significant problems for patenting new innovations and new discoveries. If generative AI is responsible for identifying new compounds and/or antibodies, can the result be patented? Under the Patent Act, an AI engine cannot be an “inventor.” Moreover, if the new discovery is based on an engine that has been educated with all of the available prior art, published knowledge and resources, then the outcome may not be truly novel and may not constitute patentable subject matter. If patent protection is not available, will bio-pharmaceutical companies turn away from generative AI to formulate the most effective and important new compound? Or – as I predict – will it be time for a new form of sui generis IP protection that balances the benefits of using AI while rewarding companies with a limited period of exclusivity.”

Kristina Simmons, Founder, Managing Partner, Overwater Ventures
The year healthcare AI stops piloting and starts producing
AI is transitioning from pilot mode into operational mode – with one study showing 22 % of healthcare organizations now use domain-specific AI tools, a 7× increase over the prior year. That means 2026 will be the year systems overhaul – diagnostics, scheduling, workflow optimization move from promise to core operations. Cost-pressures, workforce shortages, and digital expectations will force systems to adopt automation and intelligence. The winners will be those building with operational adoption in mind, not just clinical novelty.

Sundar Subramamian, CEO of Zyter/TruCare
Telehealth Becomes the Front Door to Rural Care, powered by AI Agents, Not Video Visits
In 2026, telehealth stops being the fallback option for rural communities and becomes the front door to the health system. The shift isn’t about more video visits. It’s about AI-orchestrated hybrid care that continuously manages a rural patient before, during, and after the encounter.
The breakthrough will come from integrating remote monitoring, automated triage agents, and virtual care teams into a seamless experience that closes care gaps and keeps clinicians informed in real time. With new CMS rural health flexibilities and a wave of omnichannel tools, telehealth finally becomes a viable operating model, not an emergency substitute.
The winners in rural health will be the systems that treat telehealth not as a channel, but as an operating system for continuous care.

Jim Szyperski, CEO, Acuity Behavioral Health
AI Can Transform Behavioral Care, but Only If the Industry Fixes Its Data First
Thoughtfully designed and implemented, AI and data-driven automation is and will be indispensable in behavioral healthcare for clinical decision support for trained staff. It is an extremely valuable tool to aggregate information that would otherwise take hours, days, weeks, to gather. IMO, it should be used solely to inform and suggest in clinical settings, and not to replace clinical decision making.
But effective use of AI/data-driven use in behavioral healthcare clinical settings requires standardized measurements being used industry wide, and that is currently far from the case in behavioral healthcare. Everyone operates their clinical environments differently, and clinical care from site to site is subjective,qualitative, resulting in little to no data that can be used for industry analysis, development of best practices, etc. In this sense, AI has become a buzzword for innovation, perhaps posturing, in behavioral healthcare, and may have the impact of increasing variability rather than creating standards.

Jordan Taradash, CEO of advanced primary care provider PeopleOne Health
AI will hone in on its purpose(s) in healthcare. After years of hype and widespread exploration, 2026 will be the year AI shifts from broad experimentation to targeted impact. Its greatest use will come from automating administrative work to free up clinicians’ time to focus on patients, while improving both virtual and in-person care with guidance and clinical decision support throughout the care journey.

Heather Trimble, Health Care Strategic Advisor at SAS
AI productivity stacks become the norm. By the end of 2026, every major enterprise will have an AI productivity stack. The same way every business today has cloud and customer relationship management (CRM), LLMs stitched into deterministic engines will run everything from marketing copy to medical billing. Generative AI gets the headlines, but deterministic AI writes the checks. Together they make the modern enterprise faster, leaner, and more inhumanly efficient. The losers will be clinging to the illusion that AI is another “tech wave.”

Owen Tripp, CEO of Included Health
Adapting to the Proliferation of LLMs
In 2026, the front door to healthcare will be an LLM, but the winners will be the platforms that combine open intelligence with deeply personal and tailored context. Consumers will increasingly turn to publicly available LLMs to understand their symptoms, decode complex conditions and build fluency in medical language before ever speaking to a clinician. This will and has already started to fundamentally change the power dynamic in care with patients arriving informed, curious and ready to engage as active participants, rather than passive recipients of care. However, general-purpose AI can only go so far and the platforms that break through will be those that can securely incorporate a member’s full medical, behavioral and financial context, including claims history, clinical records and communication preferences to then translate that into actionable and personalized guidance. Because smaller companies will likely struggle to compete in this environment, which requires massive, secure and real-time data pipelines with complex predictive workflows, scaled virtual care organizations will be critical partners across the ecosystem. Beyond being care providers, these organizations will be trusted intelligence layers that enable the delivery of a complete, contextualized medical experience.

Engy Ziedan, Chief Science Officer and Co-Founder at Protégé
Benchmarking The Next Leap in AI
People ask what the next big leap in AI will be, and I don’t think it’s another model release. It’s a reckoning with how we measure and evaluate progress. By 2026, we’ll see growing recognition that many of the benchmarks defining AI performance today are too narrow and too far removed from the complexity of the actual world where these models are going to be used. This will also lead to the increasing need for healthcare data from real-world scenarios from around the globe.
For years, we celebrated when models surpassed humans at tasks like chess, Go, or textbook-style medical exams. But outperforming on those metrics doesn’t translate into real-world utility or reaching the full potential of what we can build. In healthcare, for example, most benchmarks test whether a model can mimic a medical resident’s textbook answers, not whether it can assist an experienced clinician making judgment calls under pressure. But we’re not there yet in having the right data that’s fully representative of these situations.
This next phase of AI development will focus less on building bigger models and more on ensuring we’re a) training with the right data, and b) measuring the right things with the right data. That means assembling the right datasets to train models in a targeted way, and then designing evaluations with data that reflects authentic human decision-making. The real breakthrough in 2026 will not come from raw intelligence, but from scientific integrity, creating transparent, statistically principled frameworks that let us understand not just what models can do, but how, when, and why they fail.