What You Should Know:
– Digital transformation strategy has accelerated as a core priority for the healthcare industry, driven by the necessity of operational resilience, personalization, and advanced AI.
– According to the fifth annual Health System Digital Transformation Survey by Chartis, 91% of health system executives agree that their organizations must undergo “fundamental change” to overcome persistent challenges and thrive in the next five years.
The Limit of Incremental Change is Reached
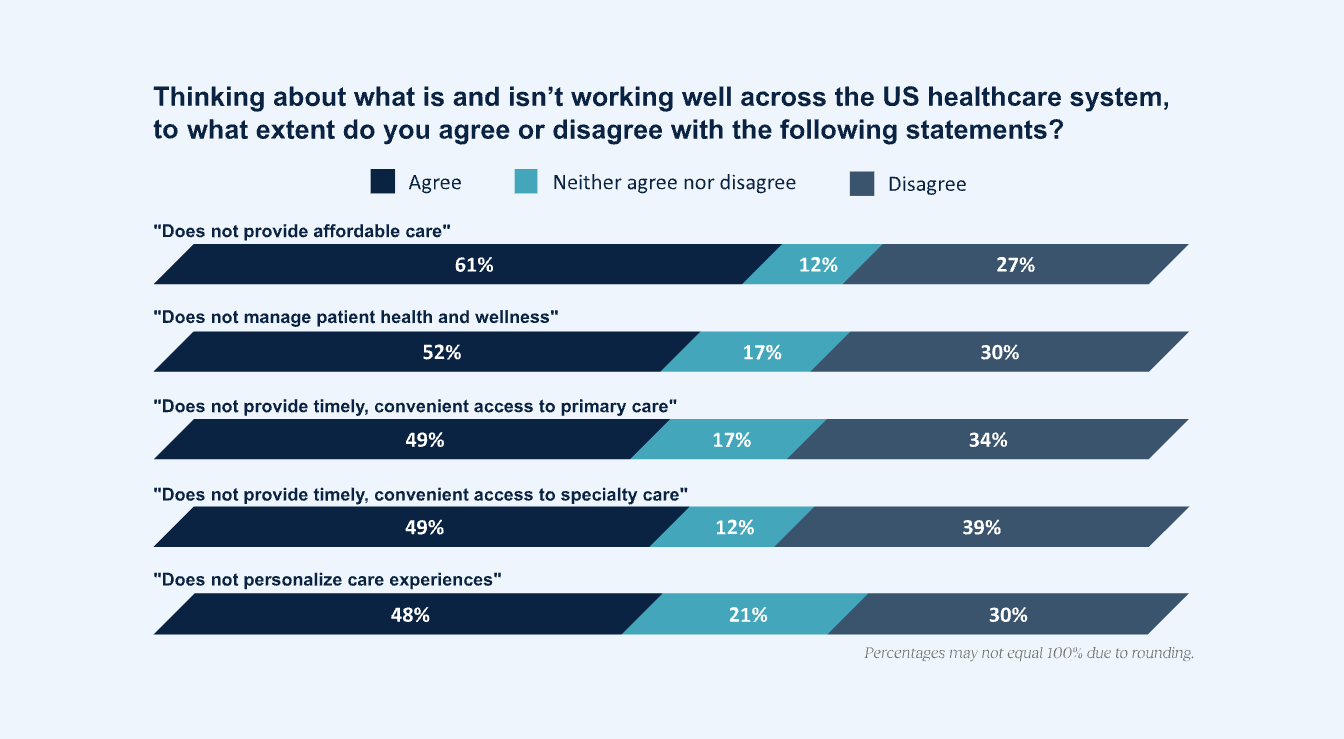
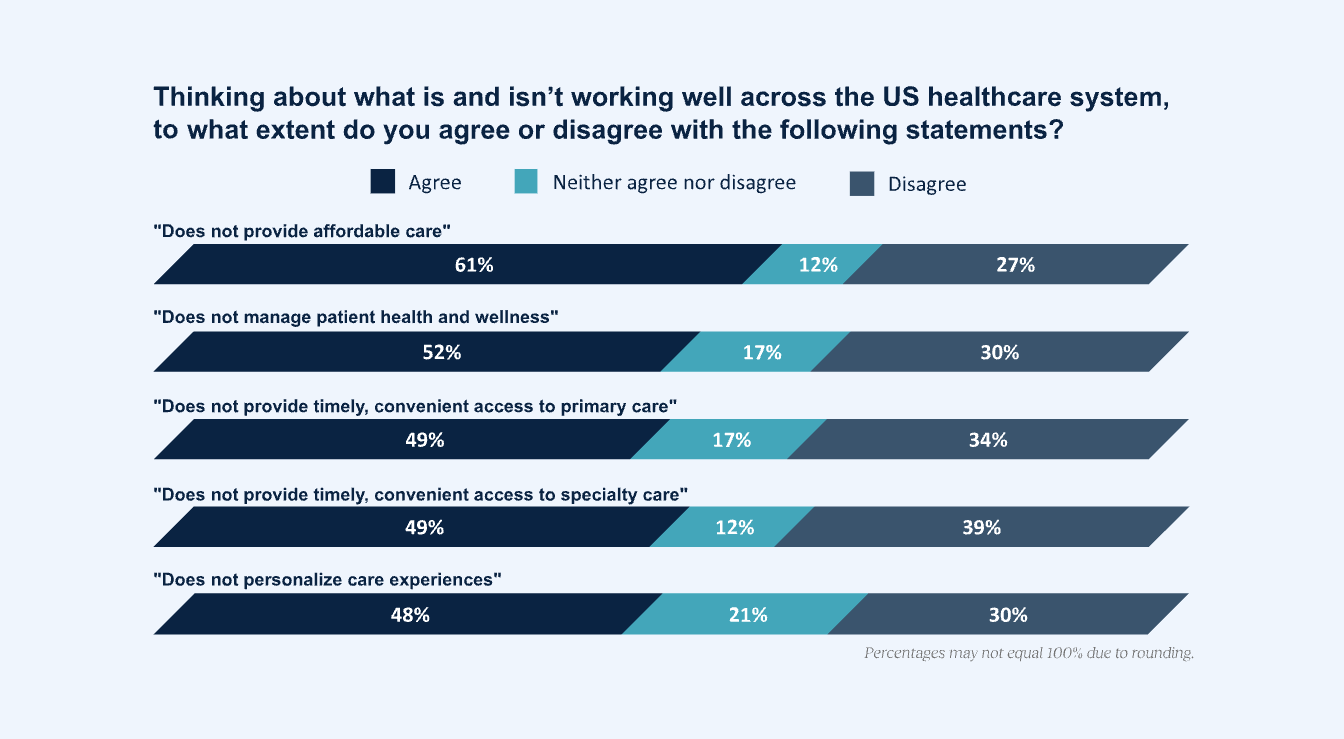
Health systems have long relied on incremental improvements to address chronic problems, but executives now acknowledge this approach has reached its limit. The challenges—which include 61% indicating care is not affordable and ~50% reporting patients lack timely access—will only worsen without significant structural transformation.
Executives are pursuing proactive models to deliver care that is more accessible, lowers cost, and provides intelligent, patient-centric services. This paradigm shift is entirely dependent on leveraging new, advanced digital and AI tools.
As report co-author Tom Kiesau, Chartis’ Chief AI & Digital Officer, notes, “We may finally be at a tipping point if 90% of healthcare executives agree on the need for fundamental change. Organizations need to capitalize on the momentum in this moment—and ensure that they are truly realizing the potential presented by AI and digital capabilities to drive needed business transformation at scale.”.
The Four Pillars of Proactive Transformation
Executives seem cautiously optimistic that they can systematically transform the reactive care delivery model using AI and digital enablement. They aim to achieve this shift through four priority domains over the next five years:
- Transforming Access: (89% prioritize digital/AI) Enabling timely, convenient, and affordable care.
- Personalizing the Patient Journey: (86% prioritize digital/AI) Engaging and guiding patients through clear care plans.
- Fitting Resources to Demand: (77% prioritize digital/AI) Accurately projecting demand and efficiently meeting those needs, particularly via Hospital at Home models.
- Serving More Patients: (75% prioritize digital/AI) Growing capacity through digitally enabled and automated care models that do not require additional clinical headcount or facility square footage.
Executives believe that by investing in advanced digital and AI tools, they can create a dynamic operating model that is faster, less capital-intensive, and capable of proactively addressing care issues upstream.
Digital Maturity Defines Competitive Advantage
The survey reveals that the key attributes defining leading health systems are shifting away from traditional metrics:
- Size is Deprioritized: Most executives agree that a health system’s size will be less of a differentiator in the future. Size alone will not insulate organizations from multiplying industry challenges.
- Digital Differentiators Win: The two greatest differentiators of leading health systems in five years will be a digital-first consumer experience and digitally enabled care. This levels the playing field, offering smaller health systems an opportunity to differentiate through strategy.
Imperatives for Strategic Execution
The path forward requires business transformation, not just process digitization. Chartis advises leaders to:
- Prioritize Proactive Investments: Align digital investments with redesign opportunities in the four major domains, focusing on transformation, not just efficiency gains in specific processes.
- Avoid Pilot Purgatory: Executives must establish discipline and clear commitment to move beyond the piloting phase. Success requires setting specific metrics for value creation, designing for scaled deployments, and integrating the technology into existing strategic initiatives.
- Build in Adaptability: Health systems must become dynamic learning organizations, applying lessons from both successful and failed implementations into future iterations.